Frequently Asked Questions (FAQs) on Fertility
Three appointments are done online via Microsoft Teams and the remaining appointments are face-to-face in the clinic.
The wait time for a New Consultation can be anything between two to six weeks but could be up to eight weeks depending on the time of year.
- Call the clinic directly to book your New Consultation at 01992-785060.
- Pre-assessment – Initially, you will need a pre-assessment appointment with the nurse. At this appointment, we will check your BMI (Body Mass Index) and do a blood test to check your AMH Level (Anti-Mullerian Hormone). The AMH blood test checks your ovarian reserve and can be done at any time in your cycle. A semen analysis will be done for all men.
- New Consultation – Once we have performed these initial tests you will then see one of our consultants remotely via Microsoft Teams approx. one week later, to discuss your results and create a treatment plan going forward.
- TIA – If the consultant has recommended fertility treatment, you will then see one of our fertility specialist nurses for an online Treatment Information Appointment (TIA) via Microsoft Teams. During this appointment, you will need to sign all your consent forms for the type of treatment you are having and plan your cycle of treatment from start to finish.
It takes approximately two to three months from start to finish. A short protocol will take around four weeks in total from starting medication to the pregnancy test result. See a typical timeline for IVF with ICSI: https://hertsandessexfertility.com/treatments/treatment-journey/
No, the AMH blood test can be done at any time of your cycle. For more info on AMH see: https://hertsandessexfertility.com/anti-mullerian-hormone-amh-test-demystified/
When undergoing treatment that involves sedation patients must have a BMI of less than 34 unless they are NHS patients. NHS patients must have a BMI of less than 30.
Egg recipients, frozen embryo transfer (FER) and IUI patients must have a BMI of less than 40 unless they will need sedation.
We can treat patients with their own eggs up until their 46th birthday, and with donated eggs up until their 51st birthday.
Eggs can be donated anonymously up until their 36th birthday and sperm can be donated anonymously up until their 46th birthday – as per HFEA guidelines.
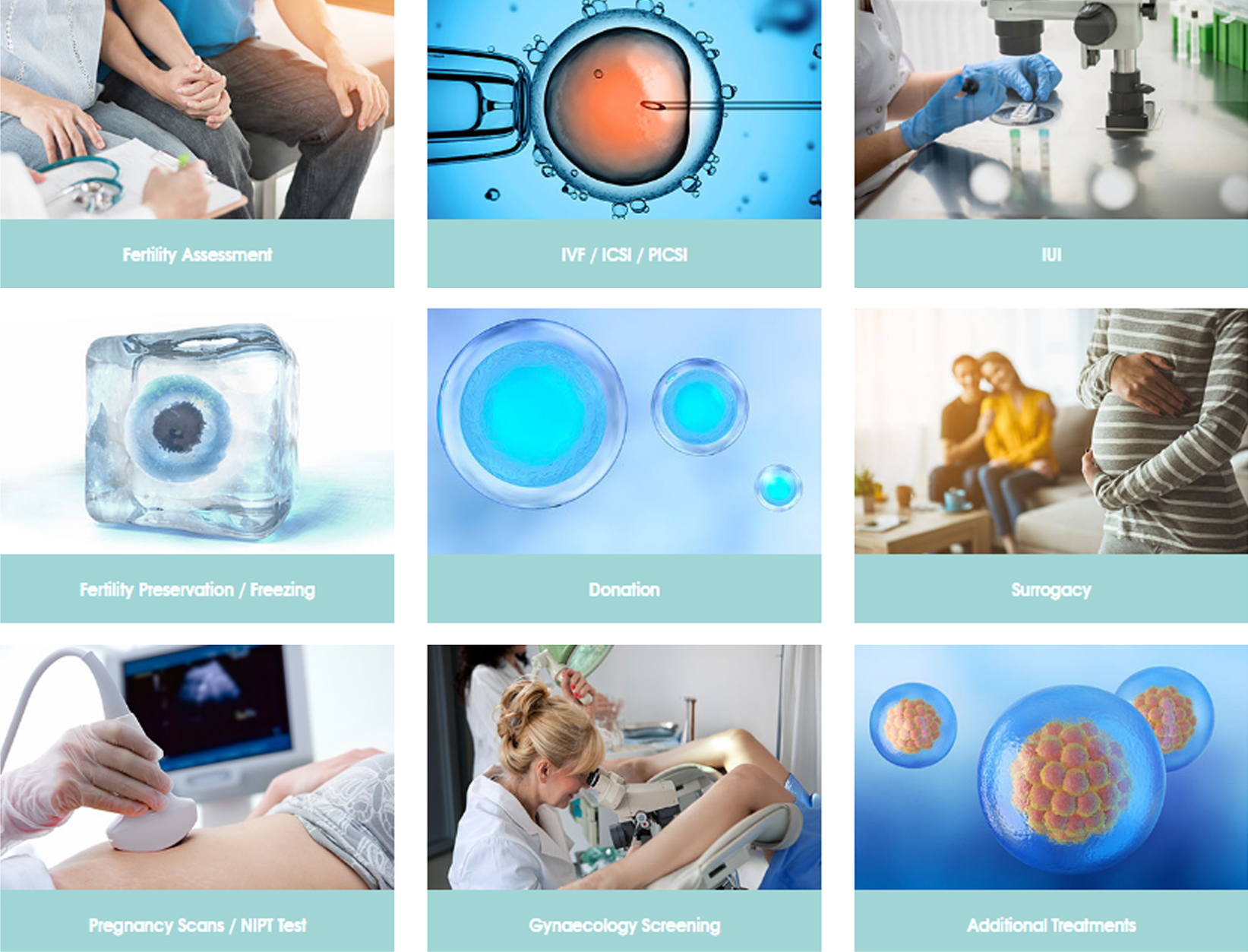
What is the difference between IUI, IVF, ICSI and PICSI and why would you choose one over the other?
With IUI, sperm is introduced into the womb by means of a small procedure at the time of the cycle when the woman is ovulating and then the egg is released naturally from the woman with the hope that the sperm and egg will meet and form an embryo.
With IVF the person providing eggs has to take medication to grow several follicles, the eggs are removed from the body during an egg collection procedure and then fertilised with the sperm in the laboratory. The fertilised egg and sperm then form an embryo which is placed back into the womb a few days later. For a same-sex female couple where the lady has normal fertility levels and patent fallopian tubes, it may be an option to try IUI first as it is less invasive and less expensive.
ICSI is a specific method used in the laboratory to fertilise the eggs. Unlike standard IVF, where the sperm and eggs are mixed together to allow the sperm to fertilise the eggs, in ICSI an individual sperm is injected directly into each suitable egg. ICSI is recommended to patients based on their medical history and test results and will be discussed with you at your new consultation appointment with a doctor.
PICSI is a very similar process to ICSI. There is an additional sperm election method which is used to choose sperm which are most likely to be mature. As with ICSI this is recommended based on your medical history and test results and will be discussed with you at your new consultation appointment with a doctor.
Costs are approximate numbers only and may vary on a case-by-case basis depending on personal circumstances and individual medical needs. Fertility treatment costs do not include medication and can be viewed on our price list: https://hertsandessexfertility.com/price-list/
Access Fertility offers patients three IVF funding packages which provide:
- A fixed cost for treatment
- The potential cost of treatment is reduced by up to a third
- Up to a 100% refund
These financial packages are offered completely independently of Herts & Essex Fertility and do not affect any clinical decisions or the quality of care that we offer during your treatment. For more info:
Patient – FBC, HIV, Hep B (Core & Surface antigen), Hep C, Chlamydia & Gonorrhea, Rubella, HB electrophoresis
Partner – HIV, Hep B (Core & Surface antigen), Hep C, Chlamydia & Gonorrhea
Not necessarily, we would not ask you to repeat certain tests you have already done, depending on the tests or when they were done. The AMH blood test remains valid for one year.
Both, patient and partner will need to be screened before commencing treatment. This is a requirement from the HFEA.
The following screening blood tests are needed for both, patients and partners:
Patient:
- Full Blood Count
- HIV
- Hep B (Core and Surface Antigen)
- Hep C
- Chlamydia
- Gonorrhoea
- Rubella
- HB Electrophoresis
Partner:
- HIV
- Hep B (Core and Surface Antigen)
- Hep C
- Chlamydia
- Gonorrhoea
These blood tests are valid for three months up until the point of egg collection and then they are valid for two years. If you don’t have an egg collection after this three-month period, these blood tests will need to be repeated again.
If you decide to have these blood tests done externally or have had them done at a previous clinic and they are in date, we will need to check that the blood tests have been performed in a UKAS Accredited Laboratory. If they haven’t, then as a clinic we cannot accept them and they will need to be done again. Treatment cannot commence until we have the results from these blood tests in place.
Yes, we would require a repeat semen analysis before embarking on treatment. This is because when assessing semen to determine its suitability for each of the treatment types available at Herts & Essex, we perform additional tests and analyses to a different criteria than is used in a standard semen analysis.
Please don’t panic, place your medication in the fridge as soon as possible if we have advised you to do so and call the clinic for further advice. It all depends on the temperature at the time and where the drugs have been stored – we can offer you further advice and instruction when you call the nursing team.
Once you have started your IVF medication you must make sure to use barrier methods of contraception when you have intercourse. We advise that you continue to use barrier methods throughout your treatment, up until your first scan following embryo transfer.
We have sperm immediately available in our sperm bank for all fertility treatments except IUI. You can also use sperm from external sperm banks such as London Sperm Bank, Xytex, and Cryos. Importing sperm from external banks can take different lengths of time depending on the bank.
Our waiting list for donor eggs is currently around six to nine months. For more information on egg and sperm donation see: https://hertsandessexfertility.com/donation/
Yes, we do offer pregnancy scans to external patients. Just call our admin team on 01992-785060 to book your scan at a convenient time.
A HyCoSy, HSG and Aqua scan are not the same thing.
Aqua Scan is a Saline Infusion Sonography that assesses the cavity of a patient’s womb. It helps to confirm or exclude things like polyps, cysts or fibroids in the uterus that shouldn’t be there and could potentially affect embryos from implanting.
HyCoSy will assess the cavity of your womb and your tubal patency. Tubal blockage is the cause of infertility in three out of ten couples.
HSG is usually done in an x-ray department by a radiologist. This is a test to assess tubal patency using a dye which is visible on x-ray. This test is not available at Herts & Essex Fertility Centre.
Yes, we do treat patients with PCOS. For more information visit: https://hertsandessexfertility.com/what-women-need-to-know-about-polycystic-ovary-syndrome-pcos/
Also see the article written by our dietitian, Alex Ballard on PCOS and Symptom Management:
https://www.alextalksdiet.com/_files/ugd/84b348_769b0e29bd7c4e7d940e021c55254959.pdf
Yes, we do treat women with Endometriosis. For more information visit: https://hertsandessexfertility.com/all-about-endometriosis-and-infertility/
No, we don’t use an Embryoscope, however we use undisturbed continuous closed culture, which is the same culture conditions as the Embryoscope.
The current survival rate for frozen embryos is 96% and the clinical pregnancy rate is 45% (average across all patient groups in 2023). For patients that have had treatment using frozen eggs, 77% of the eggs survived the freeze-thaw process and those that went on to have an embryo transfer had a clinical pregnancy rate of 55%, (across all patient groups in 2023 using either their own, or donor, frozen eggs), which is in line with published rates from other clinics. Data as of 31 December 2023
Yes, we do. Please call the clinic to speak with one of our egg donation specialists so we can give you detailed information about this. Factors to consider when looking at egg donation and egg sharing are:
- Aged between 18 and 35
- AMH of 15 or above
- Fit and healthy within normal limits of weight and height
- No family history of inherited diseases, genetic disorders or any serious mental health issue
For more information on egg donation and egg sharing visit: https://hertsandessexfertility.com/donation/egg-donation/
We do offer Karyotyping / genetic testing, but only to patients who are registered with us for treatment at the clinic.
More information about the COVID-19 vaccination during fertility treatment and pregnancy can be found here:
https://bit.ly/BFSCovidFAQ
https://bit.ly/COVIDvaccineRCOG
https://bit.ly/NHSCovidVaccinePregnancy
Yes, your partner can attend all your appointments with you.
You can have your hair colored whilst having treatment. You are unable to have your hair dyed once you have had your embryo transfer and through the first trimester of pregnancy.
Yes, you can go to a spa and have a massage whilst having treatment. After egg collection, it would be advisable to avoid these for one week due to the increased risk of infection.
There’s little research on using saunas, Jacuzzis, hot tubs and steam rooms during pregnancy. But it’s advisable to avoid them because of the risks of overheating, dehydration and fainting. You’re likely to feel warmer than normal during pregnancy.
Please check with your therapist as some essential oils used for massage are not safe to use in early pregnancy.
Yes, you can have a tattoo during your treatment. However please bear in mind any procedure like this can increase the risk of infection. We do not advise you to have a tattoo after your embryo transfer.
Once pregnant, although the risk is small, it is recommended that you wait to get a tattoo until after your baby is born. Little information is available about the safety of skin dyes used for tattooing during pregnancy. It is possible that the chemicals in the dye might affect the development of the baby during the first 12 weeks.
As a clinic, we don’t offer advice on complementary therapies such as acupuncture of reflexology. We ask that you do your own research and make an informed decision on whether you think this will help/benefit your treatment.
Should you wish to consider any of these alternative therapies, you could find more information about them on the HFEA website: HFEA Complimentary and Alternative Therapies
Alternatively, if you are particularly interested in acupuncture, you could visit The British Acupuncture Council (BAcC) website and search for a registered acupuncturist using your postcode.